Pediatric Specialty Day

We invite you to join us on a journey beyond the fundamentals, delving into the intricacies of pediatric hand and upper extremity therapy. This specialized course promises an exploration of unique diagnoses, innovative treatments and the myriad triumphs and challenges inherent in the realm of pediatric hand therapy.
Whether you're a seasoned practitioner seeking to deepen your expertise or a newcomer eager to expand your knowledge, ASHT Pediatric Specialty Day is your gateway to a comprehensive understanding of the evolving landscape of pediatric hand therapy.
The theme for this year’s meeting is “Blaze a New Trail: Embracing our Future, Committing to Sustainability." This carries forward our history of sharing knowledge and expertise while highlighting the steps forward to sustain us as a profession and organization. This is also an opportunity to showcase innovations in upper extremity care that are transforming the way that we approach rehabilitation, enabling us to deliver efficient and effective care for our patients.
Pediatric Specialty Day will be held as a full day of programming the day before the start of the ASHT Annual Meeting. Registration will be available for purchase on its own or as an add-on to the full conference package.
Emily S. Ho, PhD, OT Reg. (Ont.)
2025 Pediatric Specialty Day Co-Chair
Meagan Pehnke, MS, OTR/L, CHT, CLT
2025 Pediatric Specialty Day Co-Chair
Registration
Registration is available for the Virtual Pediatric Specialty Day only or select a specially priced bundle and add the Annual Meeting to your registration. Select one of these options to register for Pediatric Specialty Day!
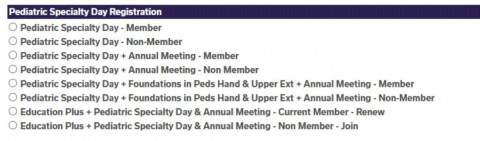
If you have already registered for the Annual Meeting and would like to also register for Pediatric Specialty Day, please contact meetings@asht.org for assistance.
Registration Category (in-person & virtual) |
Total |
| Pediatric Specialty Day - Member Full (Includes Registration to Pediatric Specialty Day Only) |
$375 |
| Pediatric Specialty Day - Non-Member Full (Includes Registration to Pediatric Specialty Day Only) |
$475 |
| Pediatric Specialty Day + Annual Meeting - Member (Includes Registration to Pediatric Specialty Day & 2025 Annual Meeting) |
$862 |
| Pediatric Specialty Day + Annual Meeting - Non Member (Includes Registration to Pediatric Specialty Day & 2025 Annual Meeting) |
$962 |
| Pediatric Specialty Day + Annual Meeting + Foundations in Pediatric Hand & Upper Extremity Rehabilitation Virtual Course - Member* (Includes Registration to Pediatric Specialty Day, Virtual Pediatric Course (Foundations in Pediatric Hand and Upper Extremity Rehabilitation) and 2025 Annual Meeting) |
$1,105 |
| Pediatric Specialty Day + Annual Meeting + Foundations in Pediatric Hand & Upper Extremity Rehabilitation Virtual Course - Non-Member* (Includes Registration to Pediatric Specialty Day, Virtual Pediatric Course (Foundations in Pediatric Hand and Upper Extremity Rehabilitation) and 2025 Annual Meeting) |
$1,205 |
| Education Plus – Pediatric Specialty Day + Annual Meeting + ASHT Dues - Current Member - Renew (Includes ASHT Dues through 2026, Registration for Pediatric Specialty Day, and 2025 Annual Meeting) |
$1,087 |
| Education Plus - Pediatric Specialty Day + Annual Meeting + ASHT Dues – Non-Member - Join (Includes ASHT Dues through 2026, Registration for Pediatric Specialty Day and 2025 Annual Meeting) |
$1,185 |
*The Foundations in Pediatric Hand and Upper Extremity Rehabilitation course includes 24 on-demand sessions as well as an online course manual. Go to asht.org for more details.
CE Hours
This continuing education activity offers a maximum of 6.5 continuing education hours or .65 CEUs.
Program:
- 8:00 AM - 8:15 AM | Welcome
-
Join the 2025 Pediatric Specialty Day Co-Chairs, Emily S. Ho, PhD, OT Reg. (Ont.) and Meagan Pehnke, MS, OTR/L, CHT, CLT as they kick off Pediatric Specialty Day!
- 8:15 AM - 9:15 AM | Resilient Foundation, Versatile Skills Symposium
-
8:15 AM - 8:30 AM | Active Movement Scale: A Critical Look at It's Benefits, Challenges, and Real-World Applications
The Active Movement Scale (AMS) is widely considered the gold standard for evaluating active movement in babies with brachial plexus birth injuries (BPBI); however, there are some real-world challenges therapists face when using it.
This presentation will examine the strengths and benefits of the AMS in clinical settings, explore the discrepancies in AMS scoring between therapists, and discuss the implications of these findings on clinical outcomes (and surgical planning). By discussing both the benefits and drawbacks of the AMS, along with the findings from our interrater reliability study, we hope to foster a critical dialogue that can lead to improved practices, consistency, and ultimately better patient care.
Learning Objectives:
1. Identify the key benefits and strengths of using the Active Movement Scale (AMS) for evaluating brachial plexus birth injuries (BPBP)
2. Analyze the challenges associated with maintaining consistency in AMS scoring and the implications for patient care and clinical outcomes
3. Develop strategies to enhance interrater reliability, including standardization of training and assessment procedures, to ensure more consistent and sustainable use of the AMS in clinical practiceSpeakers: Lindsey Williams, OT, CHT | Ashley Pittman, OTR, CHT
8:30 AM - 8:45 AM | Congenital Hand Conditions: Three Common Diagnoses
Congenital hand conditions are commonly seen by hand surgeons and therapists. We will review some common diagnoses and discuss the roles of surgeon and hand therapist for each. Photographs and case examples will be used to highlight surgical techniques, types of orthoses, therapeutic activities, and modifications for activities of daily living.
Learning Objectives:
1. List 3-5 congenital hand conditions commonly seen by pediatric hand surgeons and therapists
2. Describe the roles of the pediatric hand surgeon and therapist in working with children with congenital hand conditionsSpeakers: Karen Ayala, MS, OTR, CHT | Hilton Gottschalk, MD
8:45 AM - 9:00 AM | Scar Tug of War: The Good, The Bad, The Ugly in Pediatric Hand Burns
Are you interested in learning more about pediatric hand burns? Have you been treating pediatric hand burns, but want to know more about treatment options? Alternatively, do you specialize in pediatric hand burns and want to discuss a complex case and treatment options? No matter your level of experience, this session is for you! We will review three different cases of varying complexity, discussing evaluation, plan of care, surgical interventions, and post-op care.
Learning Objectives:
1. Discuss assessment of pediatric hand burn injury with varying complexities and the impact on function in the growing hand
2. Provide an understanding of the impact of growth and developmental progression on wound care and scar tissue and outcomes in pediatric burn care
3. Describe therapeutic techniques utilized throughout wound care and post-surgical care from initial assessment through scar maturation in three different cases of varying complexitiesSpeaker: Nichole Schiffer, MOTR/L, BCP, CHT, BT-C
9:00 AM - 9:15 AM | Q&A
- 9:15 AM - 10:15 AM | Climbing New Heights, Advanced Clinical Skills Symposium
-
9:15 AM - 9:30 AM | A Picture is Worth a Thousand Words: Using Ultrasound to Examine Effects of the Sup-ER Orthosis on Glenohumeral Joint Alignment in Infants with Brachial Plexus Birth Injury
Infants with brachial plexus birth injury (BPBI) are at risk for abnormal glenohumeral joint positions and dysplastic changes in joint surfaces. While early therapeutic strategies to mitigate glenohumeral dysplasia have been proposed, little evidence is available to support their effectiveness. Through this session, participants will be introduced to ultrasound imaging as a modality to examine glenohumeral joint morphology in infants with BPBI. The effects of the Sup-ER orthosis on joint alignment will be presented and discussed using ultrasound data to assist therapists with clinical decision-making.
Learning Objectives:
1. Identify typical infant glenohumeral joint alignment on static ultrasound images
2. Determine atypical glenohumeral joint alignment using alpha angles on static ultrasound images for infants with BPBI
3. Describe factors that could influence optimal glenohumeral joint alignment in the Sup-ER orthosis for infants with BPBISpeaker: Sarah Lewis, PT, DPT, PCS
9:30 AM - 9:45 AM | DAFRA for Pediatrics: Play Activities for Exercise After Nerve Transfer
Nerve transfer surgery techniques in young infants and toddlers with brachial plexus injuries are progressing. It can be challenging as a therapist to develop post-operative protocols and treatment plans. Not all children have a perfect result after nerve transfer surgery. Not all children regain all motions on their own. We have developed a program for young children based on the DAFRA nerve transfer rehabilitation for adults. We will explore case studies for different nerve transfers and play activities encouraging functional movements that target the donor and recipient nerves for these very young kids who cannot follow a set, strict exercise protocol. Participants will leave with ideas to take back and implement immediately with this population of children.
Learning Objectives:
1. Discuss the DAFRA protocol as designed for adults with nerve transfer and apply similar principles for the treatment of children
2. Explore examples of activities appropriate for infants and toddlers to elicit the desired movements after nerve transfer surgery
3. Develop a novel play-based activity that targets specific upper extremity functionsSpeaker: Ann Marie Feretti, EdD, OTR/L, CHT
9:45 AM - 10:00 AM | Using an Evidenced-Based, Creative Approach to Treat Elbow Fractures and Dislocations in the Pediatric Population
This presentation will briefly review the basic structures of the elbow and common elbow fractures in the pediatric population. It will differentiate healing and progression of a pediatric versus the adult population. It will highlight pediatric-centered interventions and progression of plan of care/protocol for patients who have sustained an elbow fracture and/or dislocation based on evidence from the literature.
Learning Objectives:
1. Demonstrate understanding of the basic anatomy of the elbow by identifying at least three relevant structures
2. Describe at least two differences between treating elbow trauma in the pediatric patient versus the adult population
3. List at least three creative pediatric friendly therapeutic treatment interventionsSpeaker: Michelle Hagenbaugh, MS, OTR/L, CHT
10:00 AM - 10:15 AM | Q&A
- 10:15 - 10:45 AM | Coffee Break & Exhibits
-
Grab a cup of coffee and visit the Pediatric Specialty Day Exhibit Hall to see the latest in pediatric therapy.
- 10:45 AM - 11:45 AM | Blazing a New Trail, Beyond Traditional Practice Symposium
-
10:45 AM - 11:00 AM | Training the Antagonist Muscles Eccentrically (TAME): A Non-operative Approach to Co-Contraction in Brachial Plexus Birth Injury
Co-contraction of agonist and antagonist muscles is vital for controlled joint movement. In children with brachial plexus birth injury (BPBI), maladaptive muscle firing patterns often develop, particularly with permanent BPBI, affecting motor control during nerve recovery. Co-contractive patterns include overactive triceps preventing elbow flexion as biceps/brachialis recover, and simultaneous activation of shoulder adductors and abductors during reaching. Non-invasive motor retraining is challenging, especially with weak or paralyzed muscles, and children tend to adopt the easiest movement patterns, making it difficult to block maladaptive behavior. Botox can temporarily denervate overactive antagonists, but it also weakens the injected muscles and is not without risk. The TAME approach proposes a non-invasive alternative to Botox or surgery by leveraging gravity and eccentric control of antagonist muscles to hopefully prevent and treat co-contraction in BPBI. Some patient may ultimately require injections or surgery, but should have access to a non-operative approach first.
Learning Objectives:
1. Identify problematic co-contraction or dynamic contractures at the elbow and shoulder in patients with brachial plexus birth injury that can benefit from the TAME (Training the Antagonist Muscle Eccentrically) technique
2. Understand how gravity can replace loss of active elbow flexion and shoulder abduction for the purpose of motor (re) training the antagonist muscle to support adaptive movement patterns
3. Understand key points of control at the elbow and shoulder when applying the TAME (Training the Antagonist Muscle Eccentrically) techniqueSpeaker: James H. Northcutt II, OTR, MOT, CHT
11:00 AM - 11:15 AM | Brachial Plexus Birth Injury: Navigating Transitions Beyond Childhood
Have you ever stopped to think about what life is like for children with brachial plexus birth injuries (BPBI) once they graduate from pediatric care? Pediatric hand therapists play a critical role in shaping their future; are we doing enough to prepare them for the journey ahead? This presentation will provide an overview of participation, pain, and health-related quality of life of young adults with BPBI. Evidence from the literature on lifelong participation in this population will be examined. Informed by a group of BPBI young adult patient partners, transitional care considerations for adolescents with BPBI will be presented. The importance of health literacy, self-advocacy, and the resilience to learn, relearn, and reintegrate BPBI during major life transitions will be discussed. In attending this presentation, pediatric hand therapists will be better equipped to support adolescents and their families for the lifelong journey ahead with BPBI.
Learning Objectives:
1. Explain the difference between participation, pain, and health-related quality of life outcomes of children and young adults with brachial plexus birth injury
2. Describe the health literacy needs of young adults with brachial plexus birth injury during the transition from pediatric to adult health care services
3. Discuss ways to foster self-awareness and self-advocacy skills in young adults with brachial plexus birth injury to support major life transitionsSpeaker: Emily Ho, PhD, OT Reg. (Ont.)
11:15 AM - 11:30 AM | Developing Hand Therapy Skills in Physiotherapists in Bolivia
Twenty-four years ago, an American pediatric hand surgeon partnered with a Bolivian orthopedic surgeon to provide free complex hand surgery for underserved children in Bolivia with congenital hand differences, tendon injuries, and burns. These "hand campaigns," as they are known, occur yearly throughout Bolivia.
One of the key components to the success of each hand campaign is training local physiotherapists on how to provide these children with skilled hand therapy services. Local physiotherapists are eager to learn and committed to supporting the hand campaign's vision and mission but lack the skills and resources to treat complex congenital upper extremity conditions and hand surgeries. This symposium is geared toward pediatric CHT's interested in working in developing countries to enhance the hand therapy skills of local physiotherapists. The methods we will discuss include one-on-one mentoring, didactic lectures, observing pediatric hand surgeries, utilizing a multidisciplinary team, and using technology to collaborate.
Learning Objectives:
1. Recognize challenges occupational therapists and physiotherapists in a developing country encounter while providing hand therapy care to patients with congenital hand differences, tendon injuries, and burns
2. Identify actions Certified Hand Therapists working in developing countries can take to enhance the hand therapy skills of local occupational therapists and physiotherapistsSpeakers: Andrew T. Bracken, MOT, OTR/L, CHT | Lana Hutchinson, CHT
11:30 AM - 11:45 AM | Q&A
- 11:45 AM - 12:15 PM | Embracing our Future, Sustaining our Profession Symposium
-
11:45 AM - 11:55 AM | Exploring Hand Therapy Ventures Through Graduate Student Projects
This presentation will provide participants with a comprehensive understanding of the doctoral capstone mentorship and its critical role in shaping the future of hand therapy. Attendees will gain insights on the responsibilities of a capstone site mentor, the benefits and challenges of mentorship, and the practical aspects of the capstone experience. The capstone process not only supports the development of future hand therapy professionals, but also enriches hand therapy practices by fostering innovation, evidence-based approaches, and advanced clinical skills. Designed for practicing hand therapy professionals, this presentation aims to enhance their knowledge of the capstone process while equipping them with the necessary tools and resources to effectively mentor Doctor of Occupational Therapy (OTD) students and embrace the future of hand therapy.
Learning Objectives:
1. Describe how mentoring doctoral occupational therapy capstone students enhances the hand therapy profession by promoting innovation, developing novel programs, and integrating evidence-based approaches
2. Recognize the key responsibilities of a capstone site mentor, the common challenges faced, and the professional and personal benefits gained through mentorship
3. Describe the significance of capstone mentorship in shaping future hand therapy professionalsSpeaker: Reeti Douglas, OTD, OTR/L
11:55 AM - 12:05 PM | A Clinical Practice Perspective on the Impact of Student Projects
This presentation will highlight the unique opportunity that student projects can provide to support our profession as pediatric hand therapists. Attendees will learn ways in which a hospital-based institution has implemented a variety of student
projects that have had a direct impact on clinical practice within specialty practice areas. Providing opportunities for future generations of pediatric therapists to participate in advancements in clinical practice, institute programs and research efforts
ultimately supports longevity within our field and instills a culture of innovation.Learning Objective:
1. Identify clinical practice, research and program development opportunities in which student projects can support clinicians and their department.
2. Apply concepts and outlines of student projects to personal practice areas to identify ways in which student mentorship may be beneficial.Speaker: Meagan Pehnke, MS, OTR/L, CHT, CLT
12:05 PM - 12:15 PM | Q&A
- 12:15 PM - 1:15 PM | Lunch & Exhibit Hall
-
Visit with exhibitors in the Pediatric Specialty Day exhibit hall. Lunch is included with Pediatric Speciatly Day registration.
- 1:15 PM - 2:15 PM | Instructional Concurrent Session 1
-
Optimizing Wound Healing and Hand Function After Hand Contracture Release
Hand contracture release is common in children with congenital differences or traumatic injuries. After surgery, specialized care is required to facilitate wound healing and support optimal positioning; to optimize hand function, support developmental skills and facilitate participation. Over time, the growing skeleton and underlying anatomy increases the likelihood of repeat contracture. Therefore, it is important to utilize interventions that maintain mobility and hand function for as long as possible. Using lecture, demonstration and simulated hands-on experiential activities attendees will learn: (1) specialized strategies specific to caring for pediatric hand wounds, (2) the benefit of using post-operative casting for hand positioning, and (3) interventions to prolong surgical outcomes and functional hand use.
Learning Objectives:
1. At the end of this session, participant will be able to demonstrate wound and skin care techniques specific to pediatrics that minimizes harm, facilitates healing and optimizes hand function
2. At the end of this session, participant will be able to choose and apply appropriate wound dressings for pediatrics that minimize harm, facilitate healing and optimize hand function
3. At the end of this session, participants will integrate knowledge of orthotics, anatomy and hand function to design safe interventions for maintenance of hand and finger position and mobility
Level: Advanced
Speaker: Tymar Fields, MOTR/L, CHT
Empowering Choices: An Interdisciplinary Model for Shared Decision-Making in Upper Extremity Cerebral Palsy Surgical Planning
Pediatric hand therapists play a critical role in shaping surgical outcomes for individuals with cerebral palsy, yet decision-making in complex cases often lacks a structured, collaborative approach. This session introduces a practical, interdisciplinary shared decision-making (SDM) model, ensuring that therapy professionals actively contribute to surgical planning alongside surgeons, physiatrists, and families.
Through interactive case discussions, video analysis, and real-world applications, attendees will learn to assess functional movement, identify patient-specific goals, and guide pre- and post-surgical interventions. The course will also explore Botox, selective denervation, tendon transfers, and muscle lengthening, providing therapists with the knowledge to advocate for evidence-based, functional outcomes.
Join us to develop clinically relevant skills, enhance interdisciplinary collaboration, and empower patients and families in making informed surgical decisions. This session offers valuable insights for any therapist involved in CP rehabilitation—helping you influence surgical planning and optimize patient recovery.
Learning Objectives:
1. Describe the principles of shared decision-making (SDM) and the roles of interdisciplinary team members, including pediatric hand therapists, physiatrists, and surgeons, in the surgical planning process for individuals with cerebral palsy
2. Assess patient-specific functional goals and movement impairments using video analysis and interdisciplinary evaluation methods to develop individualized treatment strategies
3. Integrate evidence-based decision-making strategies to evaluate and prioritize surgical and non-surgical interventions, ensuring alignment with patient and family goals for optimizing functional outcomesLevel: Intermediate
Speakers: Aviva Wolff, EdD, OTR, CHT | Dara Jones, MD, FAAPMR
Girls Just Want to Have Fun: Safely Returning Pediatric and Adolescent Female Athletes to Play
Sports participation continues to rise in the youth female population resulting in increases in acute and overuse upper extremity injuries leading to time away from play and loss of sport’s skill development. The upper extremity therapist requires additional specialized skills to provide optimal care for these patients. This session will discuss the evaluation and treatment of the pediatric and adolescent female’s upper extremity injuries and the influence of hormones, developmental physiology and psychology. Case examples will be utilized to illustrate the recovery strategies from the evaluation to the return to sport testing and programming.
Learning Objectives:
1. Describe the influence pediatric and adolescent female physiology on rehabilitation, exercise programming and sports performance
2. Discuss age-specific and sport-specific evaluations throughout the pediatric to adolescent female lifespan
3. Identify acute and overuse upper-extremity injuries in pediatric and adolescent athletes and appropriate rehabilitation to prepare for return to sportLevel: Advanced
Speakers: Michael Mueller, OTR/L, CHT | Alexandra Vertus, MS, OTR/L, CHT
- 2:15 PM - 2:30 PM | Transition Break
-
- 2:30 PM - 3:30 PM | Instructional Concurrent Session 2
-
Pain Talk: Age-Appropriate Approaches for Pediatric Pain Education
Complex pain impacts the entire family, and physical and occupational therapists who work closely with these families have the opportunity to make a significant difference in their understanding of pain and how they facilitate function at home. Each therapist has their own metaphors and stories that assist with connecting to patients at each phase of life and guide them through difficult and painful situations. This course offers the opportunity to share these metaphors with other therapists and learn new ways to connect to these young patients. Through demonstrations and collaborative discussions, attendees will gain new insights on how to connect with young patients and enhance their confidence in treating complex pain conditions.
Learning Objectives:
1. Choose an appropriate metaphor to explain the sensitive nervous system to a patient under the age of 7
2. Formulate a treatment plan including pain neuroscience education for a teenage patient presenting with a referral for chronic wrist pain
3. Relate biological, psychological, and social factors to a 17-year-old patient presenting with complex painLevel: Intermediate
Speakers: Hannah Gift, OTR/L, CHT, COMT UE, CEAS | Alyssa Phillips, CScD, MOT, OTR/L
Complex Traumatic Injuries of the Pediatric Hand: A Multidisciplinary Treatment Approach
Caring for the pediatric population can be difficult, daunting and challenging, yet it is extremely rewarding. This population is our future and caring for them with the goal in mind that these children will and can do big things is of utmost importance. In this presentation, we will discuss case examples of mangled hands with treatment including surgery and rehab. We will highlight the specifics of the rehabilitation program and the importance of a multidisciplinary care team for this population.
Learning Objectives:
1. Gain an understanding of the multi level effect that a traumatic hand injury in the pediatric population has on the child, family, future and care team
2. Delineate the rehab treatment algorithm for pediatric patients with mangled hand injuries.
3. Understand the imperativeness of a multidisciplinary team and how close communication with the surgeon and other MDs involved in the case for total care of the patient
3. Attendees will be able to strategize and identify fitting orthoses for various stages of treatment for pediatric patients with mangled hand injuries. We will discuss orthoses that provide protection, immobilization and mobilization when appropriate as well as orthoses that allow for wound healing particularly for wounds with a lot of exudate.Level: Intermediate
Speakers: Alta Fried, MS, OTR/L, CHT | Shaun Mendenhall, MD
Common Peripheral Nerve Injuries Associated with Pediatric Upper Extremity Fractures
Peripheral nerve injuries occur commonly with pediatric upper extremity fractures. This surgeon/therapist co-presentation will highlight common pediatric upper limb fractures and associated nerve injuries. Clinical examination and advanced diagnostic test options will be reviewed. Conservative and surgical management will be presented with case study examples, photographs, and/ or videos to enhance the learning experience.
Learning Objectives:
1. Review the categories of nerve injuries and the prognosis for recovery
2. List the nerve injuries that occur commonly with pediatric upper extremity fractures
3. Understand the rationale for conservative and surgical management of pediatric upper extremity peripheral nerve injuries that occur with fracturesLevel: Intermediate
Speakers: Karen Ayala, MS, OTR, CHT | Hilton Gottschalk, MD
- 3:30 PM - 3:45 PM | Coffee Break & Exhibit Hall
-
Chat with exhibitors in the Pediatric Specialty Day exhibit hall and grab a cup of coffee.
- 3:45 - 4:45 PM | Strengthening Evidence-based Practice: Pediatric Protocols
-
This interactive panel session will review pediatric hand therapy protocols for non-operative and post-operative patients. Our panel of experts will highlight three protocols from their institutions including intra-articular fractures, syndactyly and camptodactyly. Attendees will be invited to engage in an in-depth discussion regarding protocols related to upper extremity fractures and congenital limb differences.
Learning Objectives:
1. Describe at least 1 technique for management of intra-articular fractures, syndactyly and camptodactyly.
2. Design a treatment plan that includes evidence-based practice for management of intra-articular fractures, syndactyly and camptodactyly.
3. Apply general protocol guidelines to management of trauma and congenital upper limb differences in pediatric patients.Speakers:
Cara Smith, PT, DPT, CHT, MSHA (Intra-articular Fractures)
Sandra Schmieg, OTR, CHT (Syndactyly and Soft Tissue Release)
Peggy Faussett, MOTR/L, CHT (Camptodactyly)
- 4:45 PM - 5:00 PM | Closing Remarks
-
Join us as we embrace the future of the pediatric therapy community!
- 5:00 PM - 6:00 PM | Reception
-
Network with fellow Pediatric Specialty Day attendees and exhibitors. Light appetizers and drinks will be served. Reception is included with Pediatric Specialty Day registration and is only open to Pediatric Specialty Day attendees.
CE Hours
This continuing education activity offers a maximum of 6.5 continuing education hours or .65 CEUs.

